I Was Told to Approve All Teen Gender Transitions. I Refused.By Tamara Pietzke
For six years I worked at a hospital that said all teenagers with gender dysphoria must be affirmed. I quit my job to blow the whistle.
I know from firsthand experience what hard times are. Though I had a happy childhood, raised as the middle child by working-class parents in Washington State, my mom died of ovarian cancer when I was 22.
After that, my family fell apart. I felt lost and alone.
I decided to become a therapist because I didn’t want anyone to go through what I had, feeling like no one on this planet cares about them. At least they can say their therapist does.
I earned my master’s in social work from the University of Washington in 2012, and I have worked as a therapist for over a decade in the Puget Sound area. Most recently, I was employed by MultiCare, one of the largest hospital systems in the state.
For the six years I was there, I worked with hundreds of clients. But in mid-January, I left my job because of what I will go on to describe.
The therapeutic relationship is a special one. We are the original “safe space,” where people are able to explore their darker feelings and painful experiences. The job of the therapist is to guide a patient to self-understanding and sound mental health. This is a process that requires careful assessment and time, not snap judgments and confirmation of a patient’s worldview.
But in the past year I noticed a concerning new trend in my field. I was getting the message from my supervisors that when a young person I was seeing expressed discomfort with their gender—the diagnostic term is gender dysphoria—I should throw out all my training. No matter the patient’s history or other mental health conditions that could be complicating the situation, I was simply to affirm that the patient was transgender, and even approve the start of a medical transition.
I believe this rise of “affirmative care” for young people with gender dysphoria challenges the very fundamentals of what therapy is supposed to provide.
I am a 36-year-old single mother of three young kids all under the age of six. I am terrified of speaking out, but that fear pales in comparison to my strong belief that we can no longer medicalize youth and cause them potentially irreversible harm. The three patients I describe below explain why I am taking the risk of coming forward.

Last spring, I started seeing a new client, who at 13 years old had one of the most extreme and heartbreaking life stories I’ve ever heard. (For the sake of clarity, I am referring to all patients by their biological sex.)
My patient’s mother has bipolar disorder and was so abusive to my patient that the mother was given a restraining order. My patient was sexually assaulted by an older cousin, by one of her mother’s boyfriends, and also once at school by a classmate. Her diagnoses include depression, PTSD, anxiety, intermittent explosive disorder, and autism. She is being raised by her mother’s ex-boyfriend (not the one who assaulted her).
The year before I started seeing her, when she was 11, she was hospitalized for talking about committing suicide. Later that year, a pediatrician diagnosed her with gender dysphoria after she started to question her gender. The pediatrician referred her to Mary Bridge Children’s Gender Health Clinic, whose clinicians recommended she take medicine to suppress her periods and that she think about starting testosterone.
Mary Bridge, MultiCare’s pediatric hospital, runs the gender clinic for minors and employs nurses, social workers, dietitians, and endocrinologists, who provide gender-affirming care, which includes prescribing hormones to young patients who question their gender. In order to get that prescription, patients first need a recommendation letter from a therapist. Because Mary Bridge is a part of MultiCare, their patients were often referred to therapists like me who were in their system.
In an April 2022 blog post, a Mary Bridge social worker wrote that the gender clinic’s referrals increased from less than five a month in 2019 to more than 35 a month in 2022. In May 2022, the clinic received a $100,000 donation from Patient-Centered Outcomes Research Institute “to study health care disparities” in transgender youth.
The clinic operates in Washington, one of the states with some of the most lenient legislation on gender transition for youth. In May 2023, the state legislature passed a law guaranteeing that youth seeking a medical gender transition can stay at Washington shelters—and the shelters are not required to notify their parents.
Because of my patient’s autism, it was difficult for us to engage in introspective conversations. During our first visit, she came over to my desk to show me extremely sadistic and graphic pornographic videos on her phone. She stood next to me, hunched over, hyper-fixated on the videos as she rocked back and forth. She told me during one session that she watched horror and porn movies growing up because they were the only ones available in her house.
She showed up to our therapy sessions in disheveled, loose-fitting clothes, her hair greasy, her eyes staring down at the ground, her face covered by a Covid mask almost like a protective layer. She went by a boy’s name, but she never raised gender dysphoria with me directly—though one time she told me she would get mad at the sound of her own voice because “it sounds too girly.” When I asked her how she felt about an upcoming appointment at the gender clinic, she told me she didn’t know she had one.
In between scrolling through videos on her phone, she told me how she cried every night in bed and felt “insane.” She described a time when she was eight years old and her mother nearly killed her sister. She remembered her mother being taken away. At times, she would “age-regress,” she told me, by watching Teletubbies and sucking on pacifiers.
When she started seeing me, she had recently threatened to “blow up the school,” which resulted in her expulsion.
I knew I couldn’t solve all of her problems, or make her feel better in just a few therapy sessions. My initial goal was to make her feel comfortable opening up to me, to make the therapy room a place where she was heard and felt safe. I also wanted to try to protect her from falling prey to outside influences from social media, her peers, or even the adults in her life.
With a patient like this, with so many intersecting and overwhelming problems, and with such a tragic history of abuse, it took our first three sessions to get her feeling more comfortable to even talk to me, and to understand the dimensions of her problems. But when I called her guardian last fall to schedule a fourth appointment, he asked me to write her a letter of recommendation for cross-sex hormone treatment. That is, at age 13, she was to start taking testosterone. Such a letter from me begins the process of medical transition for a patient.
In Washington State, that’s all it takes—a few visits with a therapist and a letter, often written using a template provided by one’s superiors—for minors to undergo the irreversible treatments that patients must take for a lifetime.
I was scared for this patient. She had so many overlapping problems that needed addressing it seemed like malpractice to abruptly begin her on a medical gender transition that could quickly produce permanent changes.
I emailed a program manager in my department at MultiCare and outlined my concerns. She wrote back that my client’s trauma history has no bearing on whether or not she should receive hormone treatment.
“There is not valid, evidenced-based, peer-reviewed research that would indicate that gender dysphoria arises from anything other than gender (including trauma, autism, other mental health conditions, etc.),” she wrote.
She also warned that “there is the potential in causing harm to a client’s mental health when restricting access to gender-affirming care” and suggested I “examine [my] personal beliefs and biases about trans kids.”
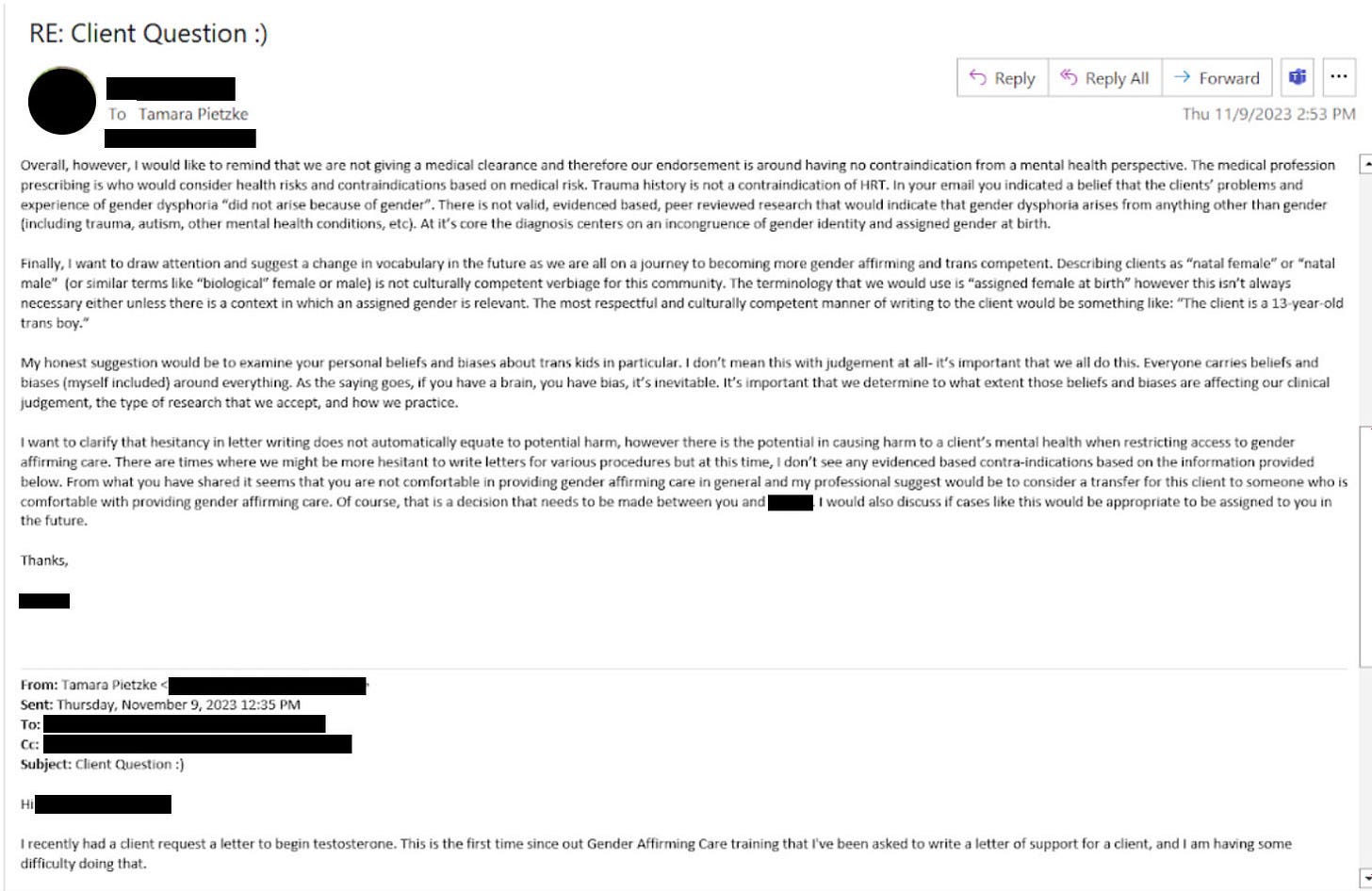
She then reported me to MultiCare’s risk management team, who removed my client from my care and placed her with a new therapist.
A risk manager’s job is to minimize the hospital’s liability, but in my case, they deemed that my concerns posed a greater risk to my client than giving her a life-altering procedure with no proven long-term benefit.

I shouldn’t have been surprised by this. Just a few months earlier, in September of last year, I was one of over 100 therapists and behavioral specialists at the MultiCare hospital system required to attend mandatory training on “gender-affirming care.”
As hard as it is to believe given my work, I hadn’t heard about gender-affirming care before that moment. I needed to know more. So each night in the week leading up to the training, I searched online for information about gender-affirming care. After putting my kids to bed, I sat glued to my computer screen, losing sleep, horrified at what I found.
I discovered that neither puberty blockers nor cross-sex hormones (testosterone or estrogen) were approved by the Food and Drug Administration as a treatment for gender dysphoria. In fact, prescribing these treatments to kids can have drastic side effects, including infertility, loss of sexual function, increased risk of heart attack, stroke, cardiovascular disease, cancer, bone density problems, blood clots, liver toxicity, cataracts, brain swelling, and even death.
While gender clinicians claim hormonal treatment improved their patients’ psychological health, the studies on this are few and highly disputed.
I found that those experiencing gender dysphoria are up to six times more likely to also be autistic, and they are also more likely to suffer from schizophrenia, trauma, and abuse.
The research also implies that the dramatic rise in these diagnoses across the West likely have a strong element of social contagion. In children ages 6 to 17, there was a 70 percent increase in diagnoses of gender dysphoria in the U.S. from 2020 to 2021. In Sweden there was a 1,500 percent increase in these diagnoses among girls 13–17 from 2008 to 2018.
Yet, countries that were once the pioneers of gender transition medicine are now starting to backtrack. In 2022, England announced it will close its only gender clinic after an investigation uncovered subpar medical care, including findings that some patients were rushed toward gender transitions. Sweden and Finland undertook comprehensive analyses of the state of gender medicine and recommended restrictions on transition of minors.
I decided—though it was potentially dangerous to my career and to me—to ask questions about the findings I discovered.
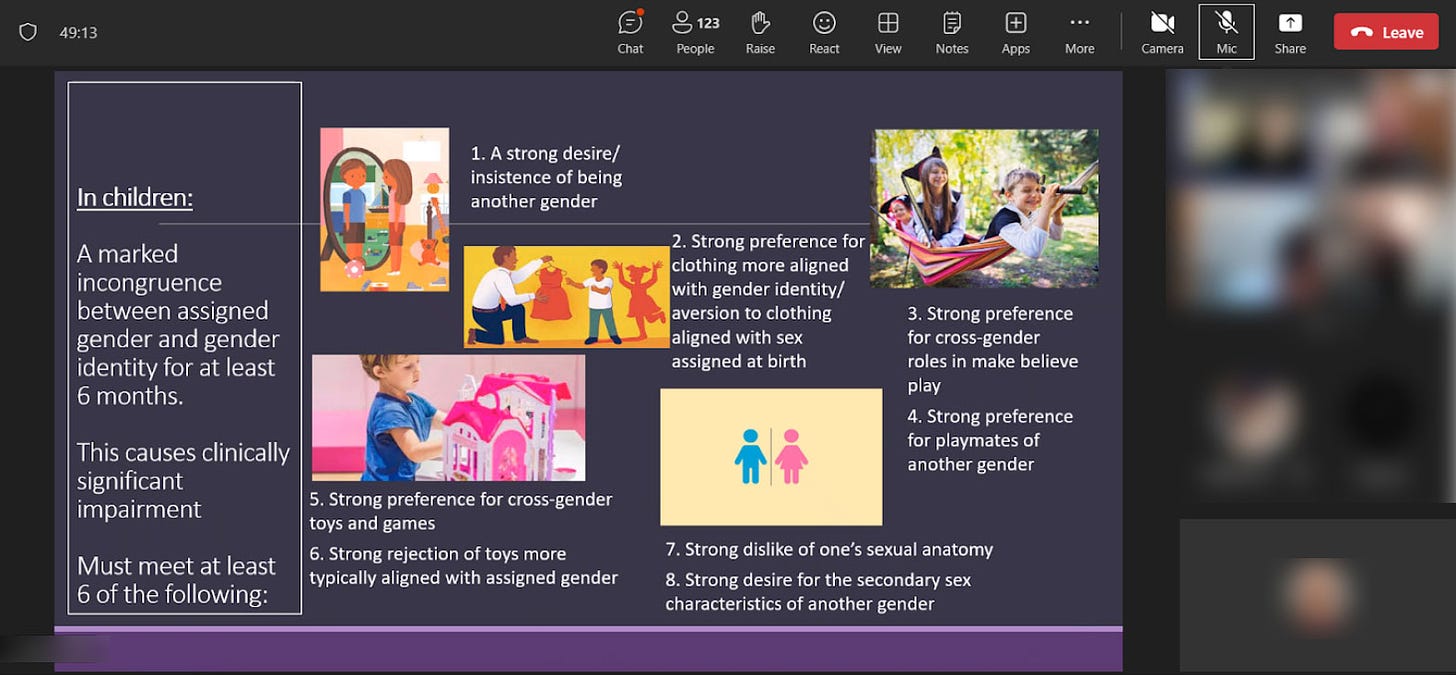
The training I attended laid out an affirming model of gender care—from pronouns and “social transition” to hormone treatments and surgical intervention. In order for children to be diagnosed with gender dysphoria, the training stated, patients must meet six of eight characteristics, ranging from “a strong desire/insistence of being another gender” to “strong preference for cross-gender toys and games.”
It was made abundantly clear to all in attendance that these recommendations were “best practice” at MultiCare, and that the hospital would not tolerate anything less.
When the leader of the training brought up hormone treatments, I shakily tapped the unmute button on Zoom and asked why 70 to 80 percent of female adolescents diagnosed with gender dysphoria have prior mental health diagnoses.
She flashed a look of disgust as she warned me against spreading “misinformation on trans kids.” Soon the chat box started blowing up with comments directed at me. One colleague stated it was not “appropriate to bring politics into this” and another wrote that I was “demonstrating a hostility toward trans folks which is [a] direct violation of the Hippocratic Oath,” and recommended I “seek additional support and information so as not to harm trans clients.”
As soon as I closed my laptop, I burst into tears. I care so deeply about my clients that even thinking about this now makes me cry. I couldn’t understand how my colleagues, who are supposed to be my teammates, could be so quick to villainize me. I also wondered if maybe my colleagues were right, and if I had gone insane.
Later, my boss reached out to me and told me it was “inappropriate” of me to raise these questions, telling me that a training session was not the proper forum. When I tried to present the evidence that caused me concern—the lack of long-term studies, the devastating side effects—she told me she didn’t have time to read it.
In retrospect, this ideology had been growing in power for a long time.
I remember in 2019 seeing signs of how gender dysphoria arose among many of my most vulnerable female clients, all of whom struggled with previous psychological problems.
In 2019, I started seeing a 16-year-old client after her pediatrician referred her to me for anxiety, depression, and ADHD. When I first met her, she had long blonde hair covering her eyes, to the point you could barely see her face. It was like she was going through the world trying to be invisible.
In 2020, during the pandemic, she told me she had started reading online a lot about gender, and said she started feeling like she wasn’t a girl anymore.
Around this time, her anxiety became so debilitating she couldn’t leave her house—not even to go to school. After taking a year off school during the pandemic, she enrolled in an alternative school for kids struggling with mental health. I was relieved that she was making friends for the first time, and seemed to be feeling a lot better.
Then she started using they/he pronouns, identified as pansexual, and replaced the skirts and fishnet stockings she often wore with disheveled and baggy clothes. Her long hair became shorter and shorter. She started wearing a binder to flatten her breasts. She tried out a few different names before settling on one that’s gender neutral.
The official diagnosis I gave her was “adjustment disorder”—an umbrella term often applied to young people who are having a hard time coping with difficult and stressful circumstances. It’s the type of diagnosis that doesn’t follow a child forever—it implies that mental distress among kids is often transient.
She came out as transgender to her family in 2021. Her mother was supportive, but her dad wasn’t. Regardless, she went to her pediatrician seeking a referral to a gender clinic.
In 2022, she went to Mary Bridge Children’s Gender Health Clinic for the first time, where the clinicians informed her and her parents that if she didn’t receive hormone replacement therapy, she could be “at increased risk for anxiety, depression, and worsening of mental health/psychological trauma,” according to her patient records. Her dad refused to start his daughter on testosterone, and so all the clinic could do was prescribe birth control to stop her period due to her “menstrual dysphoria,” or distress over getting her period. Which is something I thought all teenage girls experienced.
Five months later, she swallowed a bottle of pills and her mother had to rush her to the emergency room.
By early 2023, my client logged on to our weekly session, which we started doing by Zoom, and she told me she identified as a “wounded male dog.” She explained to me that this was her “xenogender,” a concept she had discovered online, which references gender identities that go “beyond the human understanding of gender.” She said she felt she didn’t have all of the right appendages, and that she wanted to start wearing ears and a tail to truly feel like herself.
I was stunned. All I could do was silently nod along.
After the session, I emailed my colleagues looking for advice. “I want to be accepting and inclusive and all of that,” I wrote, but “I guess I just don’t understand at what point, if ever, a person’s gender identity is indicative of a bigger issue.”
I asked them: “Is there ever a time where acceptance of a person’s identity isn’t freely given?”
The consensus from my colleagues was that it wasn’t a big deal.
“It sounds like this isn’t something that’s ‘broken,’ ” one colleague wrote me back, “so let’s not try to ‘fix’ it.”
“If someone told me they use a litterbox instead of a toilet and they were happy with it and it’s part of their life that brings them fulfillment, then great!” she continued. “I might think it’s weird, but then again, not my life.”
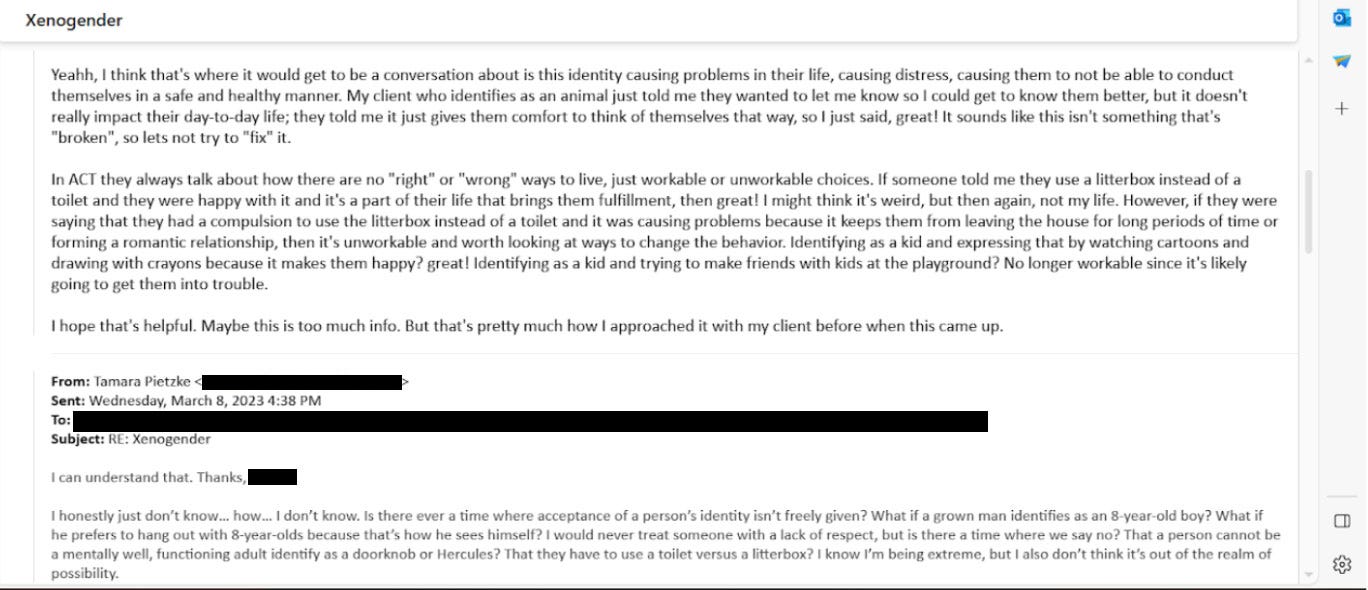
I was baffled and alarmed by her unquestioning affirmation. At what point does a change in identity represent a mental health concern, and not something to be celebrated and affirmed? Fortunately, my client never brought up her “xenogender” again. She also isn’t on testosterone due to her father’s disapproval. So I kept these thoughts to myself, and ultimately, in order to keep my job, I let it go.

Another female patient, who transitioned as a teen, serves as a warning of what happens when we passively accept the idea that gender transition will entirely resolve a patient’s mental health issues.
This client, who I started seeing in 2022, is now 23 and rarely leaves the house, spends most of the day in bed playing video games, and envisions no path to working or functioning in the outside world due to a variety of mental health problems. In 2016, this patient was diagnosed with autism, anxiety, and gender dysphoria. Later the diagnoses grew to include depression, Tourette syndrome, and a conversion disorder. In 2018, at age 17, the Mary Bridge Gender Health Clinic prescribed testosterone, despite the fact that this patient is diabetic and one of the hormone’s side effects is that it might increase insulin resistance. The patient’s mother, who has another transgender child, strongly encouraged it.
This patient now has a wispy mustache and a deepened voice, but does not pass as male. It turns out that testosterone, which will be prescribed for life, did not relieve the patient’s other mental illnesses.
My biggest fear about the gender-affirming practices my industry has blindly adopted is that they are causing irreversible damage to our clients. Especially as they are vulnerable people who come to us at their lowest moments in life, and who entrust us with their health and safety. And yet, instead of treating them as we would patients with any other mental health condition, we have been instructed—and even bullied—to abandon our professional judgment and training in favor of unquestioning affirmation.
I am speaking out because nothing will change unless people like me—who know the risks of medicalizing troubled young people—blow the whistle. I am desperate to help my patients.
And I believe, if I don’t speak out, I will have betrayed them.

Tamara Pietzke is a therapist based in Washington.
Comments are closed.
