Hydroxychloroquine, a year later, 3 times higher survival rate. Trump was right.
The world faced the greatest global health crisis in one hundred years, but it’s taken a whole year to write up a small study that shows hydroxychoroquine could improve the survival rate of people on ventilators by a factor of three, and that the dose matters.
If anyone says “but this is not a big study”, that’s exactly my point. Why is it so hard to get a large study of a drug that was already known to be useful against SARS-1 fifteen years before SARS-2 arrived. A drug that even the President of the US was talking about in the earliest days? In January 2020 we already knew that the three drugs that were “fairly effective” were Remdesivir, Chloroquine and Ritonavir. On February 13, the South Koreans were already recommending hydroxychloroquine and telling us the anti-virals should be “started as soon as possible”. We had that head start, we threw it away.
Apparently the kings-of-compassion in the commentariat would rather see deaths than admit Donald Trump was right. And the experts in Pharmaceutical Giants only cared about the profit line.
And so it comes to pass, finally, that we find out what happened to 255 patients in May 2020 who were treated for Covid in a hospital in New Jersey. Sadly, 78% or 201 patients are described as “expired” — as if they reached their use-by dates. It was that bad. Just 54 survived. Only 3.5% “walked out of the hospital”. These were very sick people.
The research team hunted through the data to try to figure out what was different about the group that survived. But mostly the “alive group” and the “expired group” were similar. The research team considered many different risk factors like their blood pressure, weight, age, and conditions like diabetes. They trawled laboriously through all the medications they were given as well. Convalescent plasma (blood from survivors) was one of the few things that helped, boosting survival by a factor of two. But one drug combination finally stood out even more and that was Hydroxychloroquine and and Azithromycin. (Essentially very similar to The Zelenko protocol).
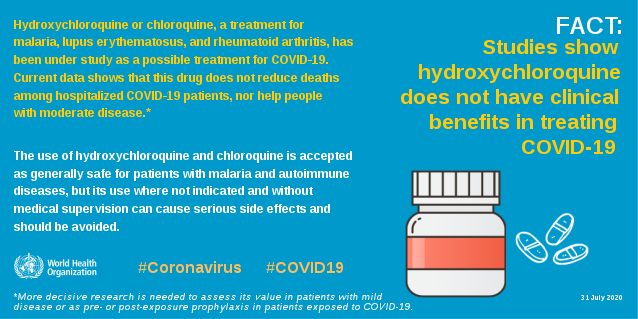
The WHO, funded by taxpayers in the West, long after these patients were saved, was working to stop HCQ from being used.
The beneficial effect of HCQ and AZ wasn’t obvious because people had received such different doses, but the higher the dose patients were given, the more likely they were to survive:
Initial lasso and Cox proportional hazard model regression analyses showed
that higher cumulative doses of HCQ were associated with a lower mortality
rate. With every natural log increase in HCQ cumulative dose, patients were
1.12 times less likely to die [p<0.001]. Accordingly, 3,000 mg HCQ cumulative dose had a survival OR = 2.46.
Hydroxychloroqine is a very unusual drug in that our bodies are very slow to get rid of it. The half life is 40 days. Therefore a repeat dose will accumulate for quite a while. So researchers started to look at the cumulative dose and it was the key:
When AZM and HCQ were given together, the association with survival
greater than when HCQ was given alone. We finally noticed that patients,
who received cumulative doses HCQ > 3,000 mg and AZM > 1,000 mg, had a much higher survival rate than all others.
The dose dependent relationship is quite telling. Only 37 patients received the highest level of 3 grams (as a cumulative dose) of HCQ and 1 g of Azithromycin. Of those, 18 survived (48%). Of the 218 patients who got less than that dose, only 36 would survive (16%).
In other words, most patients just didn’t get a high enough dose.
Patients receiving three grams of hydroxychloroquine, and one gram or more of Azithromycin had 3.26 times lower risk of dying. And the researchers then figured that dose per bodymass weight could also be important. They found that people need a dose higher than 80mg/kg. This is hardly a surprise, since nearly all medicines known to man are dished out on a per kilo basis. The bigger mystery is why other studies did not use HCQ on a per kilo dosage?
Despite all the warnings, they found no evidence that HCQ caused the longer QT Boundary side effect that the FDA worried about. Though they also note that the FDA itself didn’t seem too concerned about this effect in 150 other medical trials, only for Covid:
On April 24, 2020, the FDA issued a warning about the possible effects of low HCQ on QTc interval (47). Since 2010, the FDA has approved over 150
clinical trials, which include HCQ treatment. The FDA did and does not
require monitoring for cardiotoxicity. In each of these trials, the total HCQ
dose and expected tissue levels are markedly higher than used or seen in
Covid patients. This discrepancy lacks logic or explanation.
This is all the more poignant given that after doctors were warned about the long QT risk they reduced doses. Even in this short trial, Smith et al noticed the effect the warnings had.
The decisions to co-administer AZM were made primarily by the ID consultants. The use of AZM with HCQ was more common in the first half of this 6-week period. During mid and late April, AZM was administered less frequently with HCQ. This decrease occurred after reports that HCQ/AZM caused QTc prolongation were published.
And marvel that weight-adjusted doses are standard practice yet no one thought to test HCQ that way?
The trials, which concluded HCQ caused QTc prolongation, did not show
that a dose-based effect. Given the weight range of hospitalized Covid
patients, it is difficult to understand how weight-adjusted dosing was not considered in these reports. At a minimum, the studies on HCQ’s effect on QTc interval in Covid patients need to be redone and the extant data reanalyzed.
The verdict was that past studies on HCQ are so worthless they need to be redone.
Comments are closed.